

Many institutions require that caffeine be avoided even if an exercise stress is planned, in case there is a need to switch to a pharmacologic stress. Caffeine and methylxanthines block the adenosine receptors on arterial smooth muscle cells, thus limiting the effectiveness of these vasodilator agents ( 4). If a pharmacologic stress test with a vasodilator such as adenosine or dipyridamole is to be performed, the patient should abstain from medications containing methylxanthines and beverages, food (such as chocolate), and medications containing caffeine for 12 h ( 2) to 24 h ( 3, 4). If the study is being done for the primary diagnosis of coronary artery disease, then sensitivity will be maximized if certain cardiac medications are withheld ( 2), though this should be done only if approved by the referring physician. Patients should wear comfortable clothing and footwear for the exercise stress portion of the examination. To limit gut activity adjacent to the heart, patients should have nothing by mouth or have only a light meal, depending on the institution's preference. The first step in ensuring an optimal study is patient preparation. Interpreting physicians must be familiar with these to ensure a proper evaluation of the study. These aspects do not arise from any limitation of the procedure itself.

Other problems, including cardiac abnormalities such as balanced ischemia and hypertrophic cardiomyopathy, are more properly classified as interpretation pitfalls.
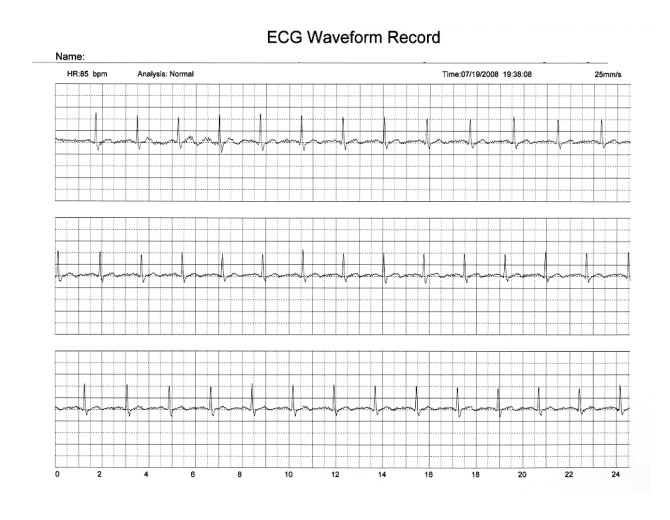
The technologist plays a key role in these steps. These must be minimized in preparation for and during the study and, if necessary, recognized and corrected after the fact. Some problems, such as motion and gating errors, are truly considered artifacts. For example, patient motion clearly originates with the patient, but the technologist has a role to recognize it and, where appropriate, to use the motion correction capabilities of the equipment to minimize its effect on the study. As depicted in Figure 1, there is considerable overlap. Artifacts and pitfalls can arise at any stage in the MPI process and can be grouped into issues related to the patient, the equipment, or the technologist. The overwhelming majority of MPI studies are now performed using SPECT and electrocardiographic (ECG) gating, which further add to the complexity of the study. Whereas MPI is a valuable diagnostic tool, it is also a complex physiologic imaging process, which exposes it to several potential pitfalls and artifacts that can limit the utility of the study. The clinical importance of MPI is in part reflected in its use, with annual double-digit growth ( 1). With its unique ability to evaluate perfusion at the cellular level and to assess perfusion at peak exercise stress, MPI plays an important role in diagnosing cardiovascular disease, establishing prognosis, assessing the effectiveness of therapy, and evaluating viability. Myocardial perfusion imaging (MPI) is a valuable tool in the management of patients with cardiovascular disease. It also presents an enormous societal burden with respect to morbidity, health care expense, and personal hardship.
#Telemetry artifact meaning how to
The reader should develop an understanding of steps to limit these factors, actions to correct them if they do arise and, when necessary, how to incorporate their influence into the interpretation of the study.Ĭardiovascular disease is the number one cause of death in North America. After reviewing this article, the reader should be familiar with the causes and the effects of these potential artifacts and pitfalls. These factors may be related to the patient (including unique aspects of the patient's heart), the nuclear medicine equipment, or the actions of the technologist. However, MPI is a complex process, subject to a variety of artifacts and pitfalls, which may limit its clinical utility. MPI plays a key role in diagnosing cardiovascular disease, establishing prognosis, assessing the effectiveness of therapy, and evaluating viability. Myocardial perfusion imaging (MPI) is an important imaging modality in the management of patients with cardiovascular disease.


 0 kommentar(er)
0 kommentar(er)
